Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Operator Perception of The Performance of Multiple Single-Use Bronchoscopes Compared to Standard Re-Usable Bronchoscope
*Corresponding author: Darrell Nettlow, Department of Pulmonary Medicine, 81st Medical Group, Keesler Air Force Base Medical Center, Biloxi, MS, USA.
Received: September 28, 2022; Published: October 12, 2022
DOI: 10.34297/AJBSR.2022.17.002333
Summary At a Glance
Single-use bronchoscopes have increased in popularity as concern for cross-contamination has increased. However, direct comparisons of the performance of these bronchoscopes to traditional re-usable bronchoscopes has been limited. In this study, we compare operator perception of re-usable and single-use bronchoscope performance in an ex-vivo model highlighting maneuverability, suction capability, and imaging processing.
Abstract
Background and objectives: Multiple single-use bronchoscopes exist on the market but have not been directly compared to each
other in terms of operator preference and overall performance. We sought to compare operator perception of the performance of
three single-use bronchoscopes to each other and a standard re-usable bronchoscope.
Methods: Operators performed a diagnostic bronchoscopy on an ex-vivo model with and without a tool in the working channel and
completed a survey regarding the performance of each bronchoscope afterwards.
Results: A total of 9 physicians completed the survey. The Olympus re-usable bronchoscope received the highest overall score (90.8),
followed by H-SteriScope (83.0), A-Scope 4 (75.2) and GlideScope BFlex (51.4). The Olympus re-usable bronchoscope was rated
highest on average in every category except maneuverability into difficult airway segments. The H-SteriScope was rated highest in
terms of maneuverability into difficult airway segments both with and without a tool in the working channel. The Glidescope BFlex
had the lowest average rating in every domain.
Conclusion: The Olympus H-SteriScope was perceived as the best performing single-use bronchoscope, followed closely by the
AMBU A-Scope. The image processing of all single-use bronchoscopes was rated as inferior to that of the Olympus re-usable
bronchoscope.
Introduction
Comparing Single-Use Bronchoscope Performance
Single-use bronchoscopes have predominantly been used as intubation adjuncts in anesthesia and for bronchoscopic procedures in the ICU [1]. As such, most studies published in the last 10 years referencing single-use bronchoscopes have focused primarily on performance in difficult intubation scenarios and have enrolled anesthesia providers [2]. One of the early studies comparing the maneuverability and perceived ease of use of a single use bronchoscope compared an early model of the Ambu A-Scope to an Olympus re-usable bronchoscope in an intubation training model [3]. Published in 2011, this study found the Ambu A-Scope to be as maneuverable as the Olympus bronchoscope for fiberoptic intubations. Despite similar intubation times and similar success rates, operators reported that the Olympus reusable bronchoscope was easier to use than the Ambu A-Scope. Subsequent studies published on the single use bronchoscopes have mostly been industry sponsored and have been limited to comparison of intubation success rates. In 2020, a survey study that specifically enrolled pulmonologists were published [4]. A total of 21 pulmonology services were surveyed regarding their perception of the quality & performance of the Ambu A-Scope 4 in diagnostic and therapeutic bronchoscopies and lavage. The Ambu A-Scope 4 was found to be acceptable for diagnostic bronchoscopy. It was rated as having a lower image quality than the reusable bronchoscope, though this did not seem to impact the ability to perform the planned procedure - 95.9% of operators were successful in that regard. More complex procedures were not attempted. This is one of the only studies comparing pulmonologists’ perception of bronchoscope performance and was limited to one disposable bronchoscope manufacturer. A smaller survey study in 2020 evaluated operator perception of a recently introduced single use bronchoscope (Olympus H-SteriScope) on an ex-vivo model [5]; in this study, operators were asked to compare this bronchoscope’s performance to their hospital system’s current single use bronchoscope. This study found that operators rated the Olympus H-SteriScope as better performing than the singleuse bronchoscopes currently used at the institution, including the Ambu A-Scope and Verathon GlideScope Bflex. No studies to date have been performed that directly compare multiple single-use bronchoscopes to the current standard reusable bronchoscope.
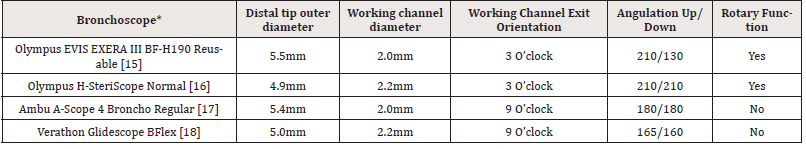
In this study, we utilize an ex-vivo model to compare operator perception of the performance of three single use bronchoscopes against a standard re-usable bronchoscope. All of the bronchoscopes chosen for this study are diagnostic bronchoscopes and possess similarly sized working channels. Therapeutic and slim/ultra-slim bronchoscopes were not evaluated. The bronchoscopes compared were as follows: Olympus EVIX EXERA III BF-H190 reusable bronchoscope (Olympus America, CO, USA), the Olympus H-SteriScope Normal (Olympus America, CO, USA), the Ambu A-Scope 4 Regular (AMBU Inc., MD, USA) and the Verathon GlideScope BFlex (Verathon Inc., WA, USA). The purpose of this study is to determine operator perception regarding the overall performance of each of these bronchoscopes as they have never been compared head-to-head.
Methods
The University of California, San Diego Institutional Review Board exempted this study from IRB review. The IRB exemption document is available upon request. Participants were recruited from faculty and fellows in the Pulmonary and Critical Care Division at our institution. Survey participants were at minimum second year fellows who had completed two or more rotations with the Interventional Pulmonology service. Participants were instructed to complete an initial airway survey with each of the four bronchoscopes. The characteristics of the bronchoscopes studied are described in Table1. The bronchoscopies were performed on an ex-vivo bronchoscopy training model (CLA-SCOPIN Bronchoscopy Model “Sick Boy”, SOMSO, Coburg, Germany). During the initial airway survey, participants were tasked with engaging four challenging segmental airways: RB1, RB6, LB1/2 and LB6. The participants then repeated the airway evaluation with alligator forceps (Olympus FB-211D.A, Olympus America, USA) inserted in the working channel to assess for changes in perceived maneuverability of the bronchoscopes when a tool was utilized (Table1).
*Each single us bronchoscope was utilized with the accompanying proprietary processing system. Both the Ambu and Verathon bronchoscopes have the processor and visualization screen in the same base. The H-SteriScope processor is a stand-alone system, and it was connected to the Olympus video monitor with a DVI cable. Bronchoscope information was obtained from each manufacturer’s website.
Immediately after completing the bronchoscopies, participants were directed to complete a 12-question electronic survey created utilizing Qualtrics survey design software (QualtricsXM, UT, USA). The survey was provided via anonymous link. Participants were instructed to rate each bronchoscope in multiple domains on a scale of 1-100. They were also asked to identify which difficult segments they were unable to engage with each bronchoscope, both with and without a tool in the working channel. A comment section was provided to allow for qualitative results to be collected.
To compare the suction capabilities of the four bronchoscopes, each bronchoscope was connected to a suction apparatus with vacuum set at maximum. The same tubing was used for each bronchoscope to ensure identical tubing length. Suction capability was tested by measuring the time needed to suction 30mL of egg white solution (Horizon Organic Egg Whites, Danone North America, USA) out of a specimen container. Three trials were performed for each bronchoscope and the results recorded.
Operator scores of the Olympus re-usable bronchoscope were used as the reference value against which each single use bronchoscope was compared. The paired t-test was utilized to assess for a significant difference between operator scores of the Olympus re-usable bronchoscope and each single use bronchoscope. This was also utilized to compare suction times between bronchoscopes. A P value of less than 0.05 was considered statistically significant. Statistical analysis was accomplished utilizing both the statistical analysis software of the Qualtrics survey system and the data analysis tool-pack of Microsoft Excel.
Results
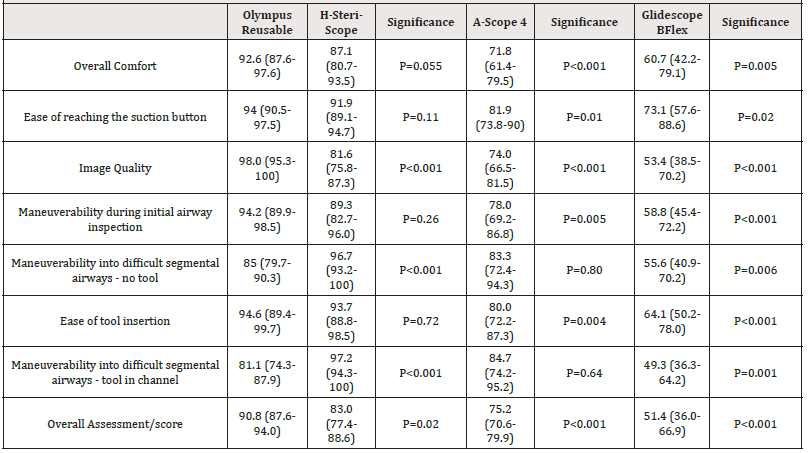
A total of 9 physicians participated in this study. All respondents completed the survey. Participant responses are reported in graphical form in figure 1. The corresponding table can be viewed in the supporting information table S1 (Figure 1) (Table S1).
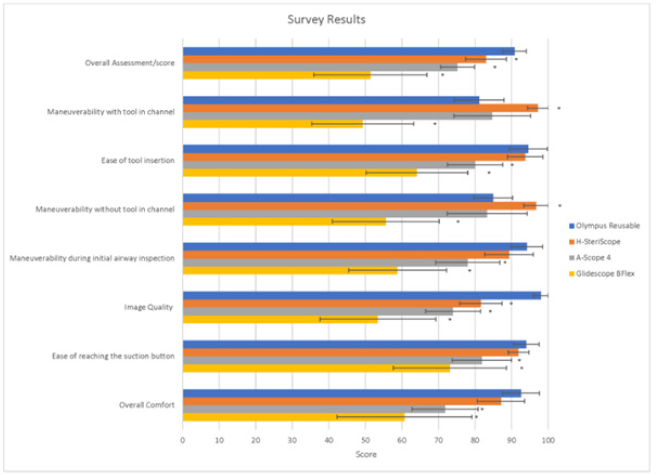
Figure 1: Survey Results. *A total of 9 respondents completed the survey. The questions were answered on a 1-100 point scale; with higher # representing a better score. The average score is listed with 95% confidence intervals displayed. An asterisk above the bar indicates a statistically significant difference in score when compared to the Olympus re-usable bronchoscope..
The Olympus reusable bronchoscope received the highest overall score (90.8), followed by H-SteriScope (83.0), A-Scope 4 (75.2) and GlideScope BFlex (51.4). The overall score of the Olympus re-usable bronchoscope was significantly higher than all single-use bronchoscopes. The Olympus re-usable bronchoscope was rated highest on average in every category except perceived maneuverability into difficult airway segments, both with and without a tool in the working channel. Image quality had the largest rated difference between the Olympus reusable bronchoscopes and the highest rated single-use bronchoscope (16.4). The difference in image quality score was statistically significant for all single use bronchoscopes when compared to the Olympus reusable bronchoscope
*A total of 9 respondents completed the survey. The questions were answered on a 1-100 point scale; with higher # representing a better score. The average score is listed with 95% confidence intervals in parenthesis next to average score.
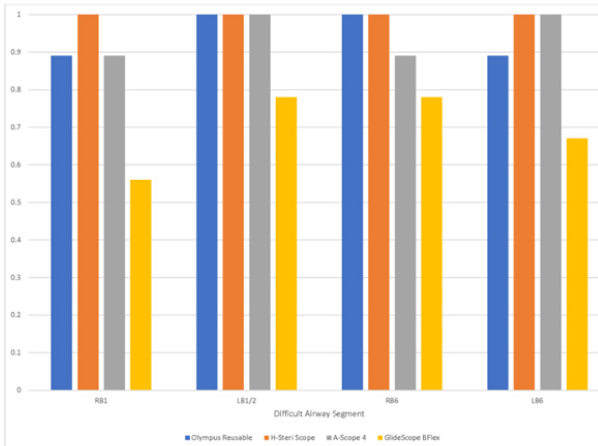
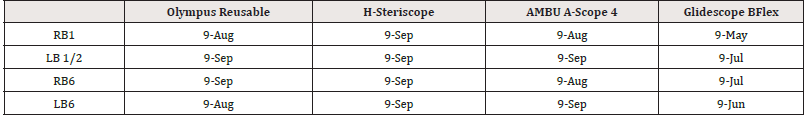
Figure 2: Percentage of respondents able to engage difficult segmental airways without a tool in the working channel. *The percentage of respondents able to access each of the difficult airway segments is presented for each bronchoscope.
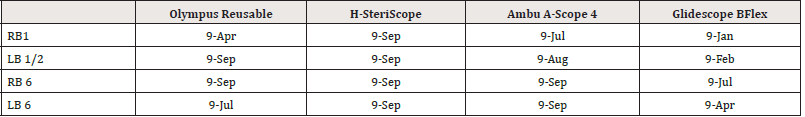
Respondents reported their ability to access each of the four proposed difficult airway segments (Figure 2,3). The H-SteriScope was able to engage the greatest percentage of difficult segments without a tool (100%) followed by the Olympus reusable bronchoscope (94.4%) and A-Scope 4 (94.4%). The GlideScope BFlex was able to engage the fewest segments (69.4%). The H-SteriScope was also able to access the greatest percentage of difficult airway segments with a tool in the working channel (100%). The A-Scope 4 was able to access a greater percentage of difficult airway segments (91.7%) than the Olympus reusable bronchoscope (80.6%) with a tool in the working channel. The GlideScope BFlex was able to engage the fewest segments with a tool in the working channel (38.9%). The tables corresponding to figures 2 and 3 can be found in supporting information, (Tables S2, S3).
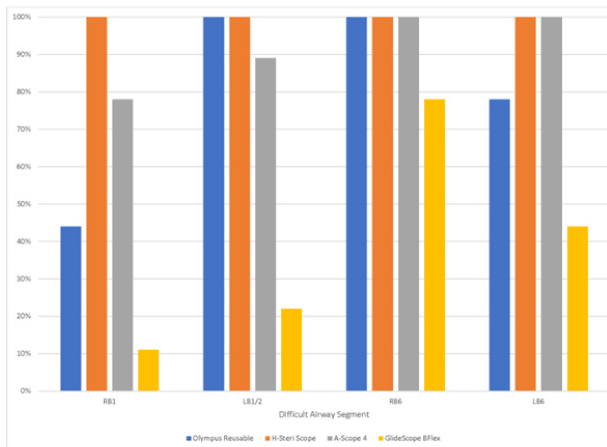
Figure 3: Percentage of respondents able to engage difficult segmental airways with a tool in the working channel. *The percentage of respondents able to access each of the difficult airway segments is presented for each bronchoscope.
Engagement of difficult segmental airways without tool in working channel. The number of respondents who successfully engaged the segment is noted the numerator; the denominator is the total number of respondents.
Engagement of difficult segmental airways with a tool in working channel. The number of respondents who successfully engaged the segment is noted the numerator; the denominator is the total number of respondents.
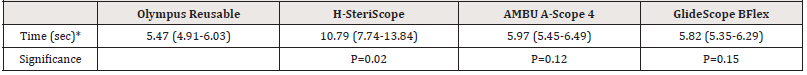
Average time to suction 30mL of fluid was similar between the Olympus reusable bronchoscope (5.47 seconds), GlideScope BFlex (5.82 seconds) and A-Scope 4 (5.97 seconds). The H-SteriScope was significantly slower to suction 30mL of fluid (10.79 seconds) (Table 2).
*The total time required for each bronchoscope to suction 30cc egg white solution. Each bronchoscope underwent three trials; average time plus standard deviation is displayed.
In terms of qualitative survey results, most respondents who chose to provide written feedback noted that the GlideScope BFlex had least ideal overall performance in terms of maneuverability and visualization. The Olympus reusable bronchoscope was the most favored given its superior image quality. The operator qualitative feedback and raw survey data is available upon request.
Discussion
Most prior studies of single-use bronchoscopes have focused specifically on their performance during anesthesia procedures such as bronchoscopic intubation and have not collected operator feedback on the performance of these bronchoscopes during routine pulmonary procedures. During the COVID-19 pandemic, there has been an increased utilization of single-use bronchoscopes to perform ICU bronchoscopies [6-8] and this has again stimulated interest in utilizing single-use bronchoscopes for pulmonary procedures [9].
In this study, we compared operator perception of three single-use bronchoscopes to the standard re-usable bronchoscope. Despite the small sample size of our study, we were able to find significant differences in operator perception of each of the single use bronchoscopes compared to the re-usable bronchoscope. Most notably, no single use bronchoscope was preferred over a re-usable bronchoscope. Overall, however, the H-Steriscope was the most favorably rated single use bronchoscope. The GlideScope BFlex fared the worst in our study population and was rated significantly lower on every domain.
Operators noted that the visualization and overall performance of the reusable bronchoscope exceeded that of all the comparator single-use bronchoscopes. However, both perception of maneuverability and ability to engage difficult airway segments favored the H-SteriScope over the re-usable bronchoscope. This performance is of particular interest given the H-SteriScope’s maneuverability was preserved both with and without a tool in the working channel. However, suctioning capability of the H-SteriScope was notably worse than any of the other bronchoscopes studied, suggesting there is not yet a consensus best-in-class device. It is worthwhile to note that the single use bronchoscope market is evolving rapidly and that in the future the image quality of single use bronchoscopes may reach that of re-usable bronchoscopes.
Tool-in-channel deflection, as defined by the difference in the angle of the working channel with and without a tool in place is of particular interest when more distal or apical targets are sought [10,11]. Our data suggests a trend toward decreased deflection in two of the single-use bronchoscopes (H-SteriScope and A-Scope 4) as indicated by the preserved percentage of difficult airway segments accessed with and without a tool in the working channel when compared to the reusable bronchoscope. While our study was not designed to make this conclusion, it could indicate an area of further research to specifically look at this characteristic.
Our study has several limitations. It is a single-center, nonblinded study with a small study sample and the bronchoscopes were utilized in an ex-vivo airway model. As such, the rated performance may differ when the bronchoscopes are employed for pulmonary procedures in patients. Specifically, the ex-vivo model does not allow comparison of the performance of each bronchoscope when blood and mucous are present in the airway; the ability of the bronchoscope’s image processer to adjust for this may differ between models. Additionally, while the ex-vivo model simulates bronchoscopy under general anesthesia, it does not simulate bronchoscopy in a patient who is coughing vigorously. The performance of each bronchoscope when significant patient motion is present may differ from their performance in the exvivo model. With that said, we have used the H-SteriScope for pulmonary procedures including alveolar lavage, trans-bronchial and endobronchial biopsies, balloon dilation and cryotherapy and in our experience this single-use bronchoscope is able to provide the visualization and maneuverability needed for most basic procedures under moderate sedation and general anesthesia. Therefore, we suspect the operator ratings we obtained in this study would translate into in-vivo use.
In the future, studies should focus on formally collecting operator perception of the single-use bronchoscopes on the market in the performance of pulmonary procedures. A standardized analysis tool would also allow for ongoing evaluation as newer models of these devices reach the market. A larger study population would allow more robust comparison to be made between systems and help hospitals and medical practices decide on which singleuse bronchoscope best fits their needs. Additionally, more in depth analysis of the cost-effectiveness of single-use bronchoscopes would better characterize the benefits or disadvantages of employing these devices in a broader clinical context [12-14].
Data Sharing Agreement
The data that supports the findings of this study are available in the supplementary material of this article
Disclosure of Competing Interests
I, Darrell Nettlow, have reviewed all authors’ ICMJE Disclosure
forms and note the following competing interests:
a. MN: Bodyvision research fund; Ion Intuitive Surgical
Consulting, Noah Medical Consulting.
b. GC: Bodyvision research fund, consulting fees from Serpex,
Pinnacle Biologics and Boston Scientific. Payment for presentations/
educational events from Medtronic, Intuitive Surgical and Cook
Medical. Advisory board for Biodesix and Prolean. Paid leadership/
fiduciary role for CHEST. Co-founding shares Restor3D.
c. The remaining authors have nothing to disclose.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was exempted from review by the UC San Diego Institutional Review Board.
References
- Marshall DC, Rucha S Dagaonkar, Chan Yeow, Anura T Peters, Siew Kin Tan, et al. (2017) Experience with the Use of Single-Use Disposable Bronchoscope in the ICU in a Tertiary Referral Center of Singapore. J Bronchology Interv Pulmonol 24(2): 136-143.
- Chan JK, I Ng, JP Ang, SM Koh, K Lee, et al. (2015) Randomised Controlled trial Comparing the Ambu® aScope™2 with a Conventional Fibreoptic Bronchoscope in Orotracheal Intubation of Anaesthetised Adult Patients. Anaesth Intensive Care 43(4): 479-484.
- Vijayakumar M, A Clarke, A R Wilkes, N Goodwin, I Hodzovic (2011) Comparison of the manoeuvrability and ease of use of the Ambu aScope and Olympus re-usable fibrescope in a manikin. Anaesthesia 66(8): 689-693.
- Flandes J, Luis Fernando Giraldo Cadavid, Javier Alfayate, Iker Fernández Navamuel, Carlos Agusti, et al. (2020) Bronchoscopist's perception of the quality of the single-use bronchoscope (Ambu aScope4™) in selected bronchoscopies: a multicenter study in 21 Spanish pulmonology services. Respir Res 21(1): 320.
- Liu L, Momen Wahidi, Kamran Mahmood, Coral Giovacchini, Scott Shofer, et al. (2020) Operator Perception of a Single-Use Flexible Bronchoscope: Comparison with Current Standard Bronchoscopes. Respir Care 65(11): 1655-1662.
- Wahidi MM, Carla Lamb, Septimiu Murgu, Ali Musani, Samira Shojaee, et al. (2020) American Association for Bronchology and Interventional Pulmonology (AABIP) Statement on the Use of Bronchoscopy and Respiratory Specimen Collection in Patients with Suspected or Confirmed COVID-19 Infection. J Bronchology Interv Pulmonol 27(4): e52-e54.
- Barron SP, Kennedy MP (2020) Single-Use (Disposable) Flexible Bronchoscopes: The Future of Bronchoscopy? Adv Ther 37(11): 4538-4548.
- Barron S, MP Kennedy (2021) Can single-use bronchoscopes help prevent nosocomial COVID-19 infections? Expert Rev Med Devices 18(5): 439-443.
- Ho E, Ajay Wagh, Kyle Hogarth, Septimiu Murgu (2022) Single-Use and Reusable Flexible Bronchoscopes in Pulmonary and Critical Care Medicine. Diagnostics (Basel) 12(1): 174.
- O Shea C, Kashif Ali Khan, Josef Tugwell, Pádraig Cantillon Murphy, Marcus P Kennedy (2017) Loss of flexion during bronchoscopy: a physical experiment and case study of commercially available systems. Lung Cancer Manag 6(3): 109-118.
- Pickering EM, Kalchiem Dekel O, Sachdeva A (2018) Electromagnetic navigation bronchoscopy: a comprehensive review. AME Medical Journal 3.
- Mærkedahl A (2020) Cost-Utility Analysis of the Ambu® aScope TM 4 Broncho Single-Use Flexible Video Bronchoscope Compared to Reusable Flexible Video Bronchoscopes. Journal of Basic and Clinical Pharmacy 11(5): 2.
- Mouritsen JM, L Ehlers, J Kovaleva, I Ahmad, K El Boghdadly (2020) A systematic review and cost effectiveness analysis of reusable vs. single-use flexible bronchoscopes. Anaesthesia 75(4): 529-540.
- Châteauvieux C, Line Farah, Emmanuel Guérot, Delphine Wermert, Judith Pineau, et al. (2018) Single-use flexible bronchoscopes compared with reusable bronchoscopes: Positive organizational impact but a costly solution. J Eval Clin Pract 24(3): 528-535.
- (2022) Diagnostic Bronchoscope (BF-H190). Olympus.
- (2022) H-SteriScopes. Olympus.
- (2021) AMBU, AMBU aScope 4 Broncho Regular.
- (2021) GlideScope BFlex Single Use Flexible Bronchoscope. Verathon.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.